These days, people stay fit and active to a much later age, but sometimes bones and joints wear out and patients need operations to restore their mobility and relieve discomfort.
To achieve this more efficiently, on the seventh floor of the Imperial College research block at the Charing Cross Hospital in London, a group of designers with very different specialties are working together to find groundbreaking advances in the world of joint replacement.
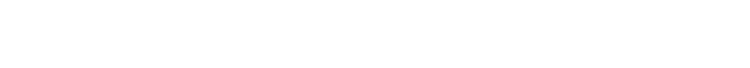
Leading the medical startup, Embody Ortho, that is driving this process is Professor Justin Cobb, orthopaedic surgeon to Queen Elizabeth II, civilian advisor in orthopaedics to the Royal Air Force, chair of orthopaedics at Imperial College London, and researcher and surgeon in the MSk Lab, Charing Cross Hospital. Cobb worked for a long time in bone cancer and moved latterly to joint replacement. After so many years of cutting away large pieces of peoples' bone, his attitude to joint replacement is to spare as much of the bone as possible.
Humans, well, we’re an active species, and motion – being alive, moving around – is an essential part of everybody’s quality of life, says Cobb. I’m curious about how people wear out, why and whether we can stop that happening.
Embody Ortho prepares 3D printed, patient-matched surgical guides for orthopaedic operations. Clever automated software, innovative design and advances in 3D printing technology combine to make highly accurate, patient-specific surgeries more reachable. Working rapidly behind the scenes, Embody uses innovative technology to take patient scans and convert them into 3D printed instruments that will be used by surgeons in operations to ensure the best outcome for the patient.
By giving the surgeon as much information as possible and reducing uncertainty in the operating theatre with the provision of a tailored set of instruments for each patient, Embody is helping to make operations faster. And they wouldn’t be able to do the work so quickly or economically without the use of a 3D printer.
3D printing is fast becoming fashionable in the design world. The technology has actually been around for decades: originally known as "rapid prototyping machines", 3D printers were used almost exclusively by the automotive industry. No one imagined the machines would be able to print anything useable. But the last decade has seen the rise of the 3D printer for jewellery, clothing, music records, sculptures of your own head, engagement rings, guns, food and more.
3D printers are being explored in the medical world too. There are a large number of technical advances in healthcare but medicine is notoriously slow at adapting to new innovations because of the need for extensive testing before implementation. Now it is increasingly common for designers to find healthcare solutions alongside doctors and engineers.
Susannah Clarke is a design-engineer specialising in medical devices. She has degrees in both engineering and industrial design and completed a PhD in computational analysis of total joint replacements. She and Cobb co-founded Embody with seed funding from the Royal Academy of Engineers in July 2012.
Clarke doesn’t have a medical background. Her engineering career began on building sites, but she felt no ownership of her work and decided to move towards products.
"I wanted to do something that was mine in a way. So I went and did a Master's in Industrial Design, which is a more creative way of making things than engineering. The design process is never perfect; that’s the difference between engineering and designing. In engineering there is a perfect solution: everything is objective, based on numbers. But design is much more subjective. It’s frustrating, but it’s much more a part of your life than engineering ever is," she says.
But the frustrating thing about product design is the nature of commercial products – they are so disposable, says Clarke. And today’s consumer market is a little bit sickening. Medical products are different, you are designing things that people really use – not buy and throw away because they are fashionable.
Unlike most design companies, the medical devices industry is filled with PhDs. Mistakes have serious consequences, and products put on the market go through huge amounts of thorough research. Before breaking into the medical device world, Clarke pursued a PhD of her own. “Then I became a sort of bio-engineering-designer person, and that brought me to Embody,” she says.
Martin Jaere joined Embody in 2013. He is a rare combination of physician-cum-designer, having completed his medical training in Norway and then a Master's in Innovation Design Engineering from Imperial College and the Royal College of Art. Jaere works as both a designer and an engineer in the MSK Lab. He was driven to working in the medical devices arena by a desire to help implement change in some of the old-fashioned systems used by doctors and health practitioners.
“The first real eye-opener came while I was a fourth-year medical student working with vascular surgeons and interventional radiologists in Trondheim, Norway. I watched how they were able to implant an artificial abdominal aorta using a minimally invasive technique with new technology, and I remember thinking, ‘This is so cool. This is what I want to get involved with. I want to make these solutions’.”
Traditionally, in the orthopaedic industry, becoming proficient at an operation meant doing a fellowship with an expert for six months to a year. But now Embody’s surgical plans are making a less experienced surgeon’s operative quality comparable to someone who does hundreds of the same operations per year.
Implants used to be really boxy, requiring huge bits of bone to be removed. But now that they are smaller and more advanced, the surgeries have become harder.
“We embed rules in the guide,” says Clarke, “and then any surgeon can access the level of skill and precision held by the leading surgeon. Everyone can have a Justin Cobb knee.”
When a patient visits a surgeon because of a painful joint, the surgeon will perform a clinical investigation and send the patient for computerised tomography (CT) scans. Embody uses these CT scans, a series of flat images, to produce one 3D model to give a visualisation of the patient’s anatomy. At this stage it is already possible to see the bone more clearly than in any operation. With these on-screen models, the Embody team can plan a surgery virtually, indicating where the implant should be placed based on the many years of research conducted within the lab. The surgeon is then sent the plan for approval.
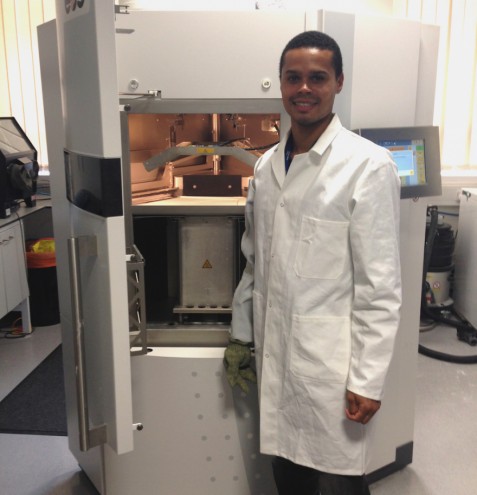
When the surgeon approves the surgical plan, a set of instruments – jigs and guides that are unique to the patient – is created in an automated process designed in-house by Dekani Fisher.
“This automation process is one of the most novel things that Embody is doing,” says Clarke, “because of the huge impact it has on the turnaround time."
Fisher uses an algorithm editor called Grasshopper to generate a new 3D model of a patient-matched surgical guide. “The information the Grasshopper algorithm takes is point data (points on the patient’s bones),” says Fisher, “which then gets turned into 3D models of the guides that we’ll 3D print.”
The process used to take more than an hour and now it takes one minute.
The surgeon will use these instruments during the operation to carry out the plan without the risk of error. These patient-specific instruments are built in the 3D printer, along with a replica of the patient’s joint from the scans.
Embody sits right at the axis of perfect need and use for a 3D printer. The Embody printer prints in a biocompatible nylon, a white polymer material, and every single set is bespoke.
“It doesn’t look beautiful but it is perfectly fit for purpose, it’s premium and it’s disposable – it only needs to be used for one surgery. There is no other way (than with a 3D printer) to make so many sets of customised instruments.”