A new bioprinted breast duct model for the study of inert breast diseases could reduce invasive treatments. It is a collaborative effort between researchers at the University of Pittsburg Cancer Institute and biomedical scientists at Carnegie Mellon University. The new method confronts the trend of overdiagnosis and overtreatment of harmless tumours. They are working together to create the world’s first 3D-printed breast ductal system to identify signs of low-risk, dormant lesions as opposed to tumours that have real potential to become aggressive.
Recent advances in mammography screening technology have been effective in finding many forms of breast cancer, but an unfortunate offshoot is that many women opt for expensive surgeries, strenuous treatments and psychological therapy to preemptively eliminate non-threatening breast tumours. The researchers between these two institutions are working to devise a better solution.
Adrian Lee, a professor at the University of Pittsburg’s cancer research department said, “Our hope is that our research will reveal novel biomarkers that will be useful for predicting which [kinds of tumours] are likely to progress. We can then offer personalised therapy to those who require intervention while reducing the overtreatment in those who don’t. This could have a major impact on thousands of women each year.”
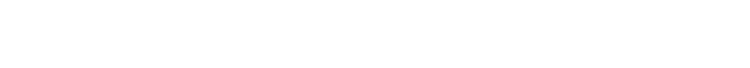
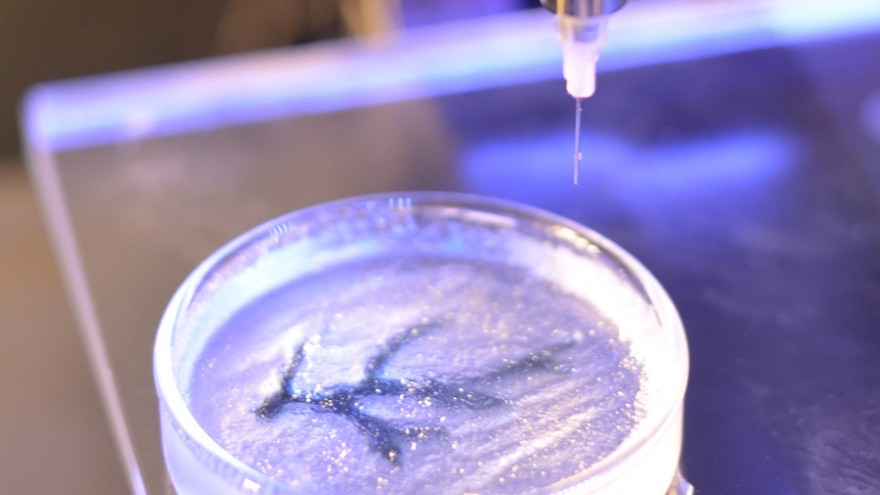
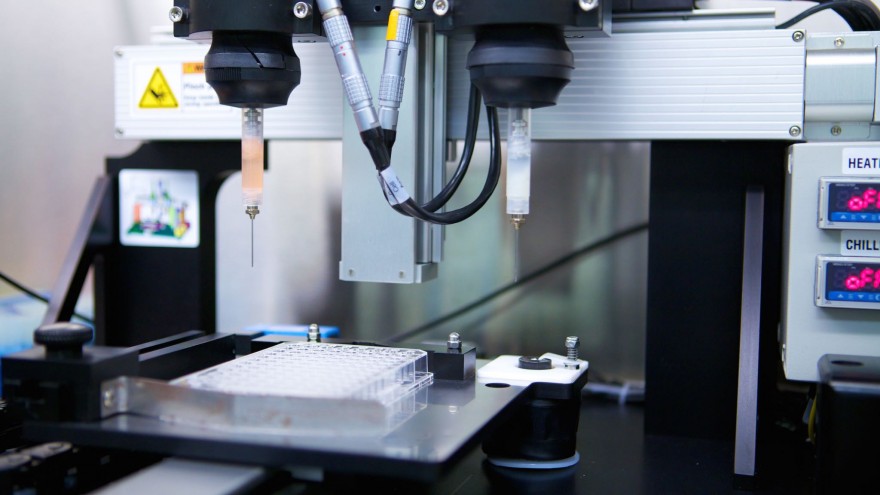
Using specialised bioprinting technology, the researchers will print a synthetic breast ductal system and grow ductal carcinoma in situ (a prominent example of non-invasive breast cancer) inside of it. The 3D-printed pseudo-organ will serve as a model for valuable study, giving experts insight on how and why certain strains of cancer become threatening while others remain totally dormant.
Adam Feinberg, a professor at Carnegie Mellon University said, “3D bioprinting is transforming how we can build tissues. By allowing us to use medical imaging data to accurately recreate complex biology, this has the potential to revolutionise bioengineering and tissue regeneration. Printing of cells and organs has been challenging because these are soft materials. Our novel technology solves this.”